Palpitations
- Dr. Mike

- 2 hours ago
- 9 min read
Summary
|
Outline
This document is provided for educational and informational purposes only and is not intended as, nor should it be construed as, medical advice. The information contained herein is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your physician or other qualified healthcare provider before starting, stopping, or changing any medication, supplement, or treatment plan. |
Background of Palpitations
A common symptom that can cause stress and anxiety among people young and old alike is palpitations or a person’s sense of beating or pounding in their chest. People can feel a sensation and describe it as a “flutter”, “skip”, “pause”, “thump”, or a variety of other ways and may or may not include a pain in the description. The common ground is that people feel something funny in their chest and it can be distressing.
Regardless of how they describe it, patients understandably will want to know what it is and how to stop it. Importantly, if you place your hand over your chest, much like if you were saying the Pledge of Allegiance (Figure 1), there are many things between the skin of your chest and skin of your back potentially associated with a “funny feeling” in the chest. Front to back, there can be sensations related to skin twitching, rib muscle twitching, heart muscle beating, esophagus twitching or spasms, and more.

What is a Heartbeat?
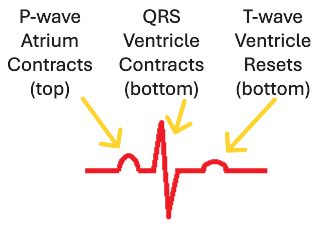
When trying to decide if the sensation is coming from the heart, it is useful to step back a bit and think about the heart. The basics of a heartbeat include an electrical signal in the atria causing the atrium to beat, which can be seen as a P wave on an EKG. Then, the electrical signal gets to the ventricles, causing the ventricles to beat, which can be seen as the QRS complex on an EKG. Lastly, the ventricles have an electrical “reset”, which can be seen as a T wave on an EKG (Figure 2).
With a little understanding of the electrical signaling of the heart and how we show it on a diagram, now you can look at four beats together. This may be called a rhythm strip and is what you can see from many different smart devices, such as watches. In the image below (Figure 3), you can see the four P-QRS-T complexes. Note the blue lines, which depict how the amount of time between the QRS complexes of two beats is relatively similar. There is often variation in the amount of time between one heartbeat and the next. When your heart beats like this, the consistency becomes something your brain blocks out and you’re less likely to pay attention to your heartbeat.

While there is usually a fairly consistent amount of between one beat and the next, there are normal scenarios where you may have different timing from one beat to the next. A common example is a premature atrial contraction, which is also known as a PAC and some patients may get enough PAC’s that they are able to feel them. With a PAC, the atrium electrically fires earlier than usual, but is usually followed by normal conduction in the rest of the heart. Given how common it is to have PAC’s, they are not usually seen as an abnormality and you don’t need to do anything to get rid of them in most cases. An example of a PAC is shown below (Figure 4). In the image below, note how the timing between beats is different, with the PAC being early, shown as a shorter time (blue line) between beats compared to the flanking beats with “normal” time between beats (green lines).

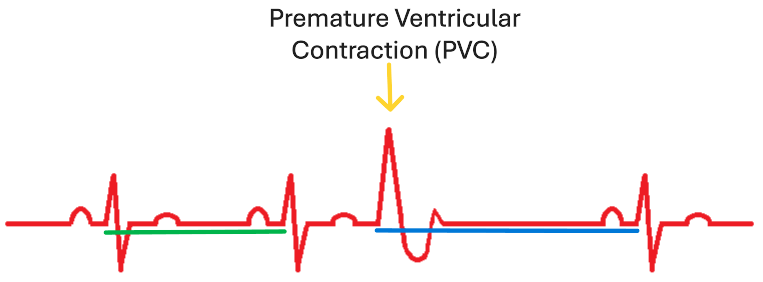
Another common cause of an abnormal heartbeat sensation is a premature ventricular contraction, or PVC. PVC’s occur when the electrical signal for a heartbeat starts in the bottom of the heart instead of the top. PVC’s can happen without any electrical activity in the atrium, so there typically won’t be a P-wave prior to the PVC’s. Importantly, there is often a “reset” of the electrical system after a PVC. As a result, the time between the PVC and the next QRS complex is often much longer than the preceding interval time between complexes, shown with the longer blue line following the PVC below (Figure 5), compared to the earlier green line. There is some thought that because there is increased time between the PVC and the beat following the PVC, there is “extra” blood in the heart and the subsequent heartbeat is much more forceful or pounding than usual. Hence, when someone is concerned they are feeling their PVC’s, what they are likely actually feeling is the beat following the PVC itself.
While it is important to know that everyone has PAC’s and PVC’s every day, most of them go without notice. Are PAC’s and PVC’s the only things that could be happening with your heart if you are feeling palpitations from your heart? No, but the other causes are far more rare.
What Can You Do?
Once a person decides they are concerned about palpitations, it is always best to review their symptoms with their physician. Why not start with a wearable device and then decide what to do? While I am certainly a fan of smart devices, and own a few myself, the important thing is that home devices may give people a false sense of security and they may dismiss important issues. Again, while PAC’s and PVC’s are common, there are conditions that can be associated with heart attacks, stroke, and, unfortunately, death which can present as palpitations. So, patients troubled by palpitations should start their workup with their physician and then, after the initial evaluation is completed under the care of their physician, then they may consider getting a home device for ongoing monitoring.
How Do You Describe the Episodes?
When a patient discusses their palpitations with their doctor, the doctor will appreciate knowing certain details about the patient’s symptoms. These details include:
What symptoms happen with the palpitations? Is there chest pain, shortness of breath, lightheadedness, dizziness, passing out, or another concerning symptoms?
How long do the palpitations last?
How many episodes happen every day/week/month/etc.?
What activities that make the palpitations better or worse?
Are the symptoms are becoming more severe or getting better?
Are there any foods or drinks (e.g., caffeine, energy drinks, and alcohol) which make symptoms worse?
Have any new physical and/or emotional stresses happened?
Have there been any medication and/or supplement changes?
What to Expect From Your Doctor?
Initially, patients concerned about palpitations will likely get an electrocardiogram (ECG/EKG). The EKG allows the physician to briefly assess if there are any concerning underlying electrical issues in the heart. Unfortunately, approximately 20% of heart attacks are silent, so it’s possible for people to have had a heart attack and not known. An EKG may help determine if there has been heart injury. An EKG may also show if there are frequent PAC’s, PVC’s, or a variety of other arrhythmias.
Presuming the EKG is normal, the patient’s doctor may then ask them to wear a monitor, which is a small, discrete device worn under a person’s shirt and attached to the left chest. A monitor is ideally worn continuously at least 3 days and preferably longer, but some people may wear them up to a month in case your symptoms are infrequent. Importantly, while wearing the device, patients should be sure to trigger the device to note an episode and then also note the symptoms present when triggering the monitor so the physician interpreting the study can look for correlations between what was felt and what was happening electrically in the person’s body. The physician will also appreciate a note as to what the person was doing at the time of the episode to look for patterns. Patients should be sure to talk to their physician ordering the device to determine if the patient should exercise while wearing the device. After the patient turns in the device, the physician interpreting it will get the results back to the ordering doctor within a few days to let them know if there were any concerning findings on the monitor.
Depending on the findings on the monitor, the patient may then have to go through a stress test, echocardiogram, or CT scan looking at the arteries of the heart. More often than not, once a person wears the monitor, no further testing is needed as the monitor can shed adequate light on what is happening electrically with the person’s heart at the time of their symptoms. There are times that a patient wears the monitor and the symptoms, such as fluttering, didn’t happen. If that’s the case, people can wear a monitor for up to a month. If that still doesn’t help, there are tiny implantable monitors that have batteries that last 3-4 years that can be placed just under the skin and which are able to monitor for concerning abnormal heart rhythms.
Clinical Science Background
A fairly recent meta-analysis of 33 studies involving 6,466 patients looked at the age distribution of atrial and ventricular ectopy (e.g., “extra beats”) and arrhythmia as determined by wearing monitors (Williams, 2020). Their review suggested there was a significant increase in atrial and ventricular ectopy with age. Importantly, when looking at a large group of healthy people who were wearing monitors, roughly 40% of healthy young adults had atrial and ventricular ectopy, with that number crossing 80% in those over 80 years old (Figure 6). In spite of the prevalence of atrial and ventricular ectopy, it is uncommon to have significant atrial arrhythmias and rare to have significant ventricular arrhythmias. So, even though many will have some degree of ectopy, it’s important to note that the vast majority of those symptoms are not associated with severe arrhythmias. That being said, it is important to see that nearly every age group can have concerning arrhythmias that warrant further evaluation. Consequently, patients should always start their evaluation of their symptoms with their doctor.

Aside from considering age, another group evaluated ventricular ectopy as a function of age and found men may be modestly more likely to have larger burdens of PVCs >5%, though the prevalence was similar between genders for PVC burden <5% (Torrado, 2024). The SAFARIS study also found men were more likely than women to have significant ventricular arrhythmia and ventricular ectopy burdens (Mannina, 2021). Williams et. al. (2020) proposed that for those under 40 years old, it may be normal to have up to 500 atrial and/or ventricular ectopic beats in a 24-hour period and that for those between 40-59 years old, it may be normal to have up to 1000 atrial and/or ventricular ectopic beats in a 24-hour period.
What Else to Consider?
People who have gone through an extensive evaluation, possibly including wearing multiple monitors, purchasing home smart devices, and gone through other cardiac testing may still struggle with palpitations. Unfortunately, common causes of palpitations unrelated to the heart includes stress, anxiety, and panic. Patients who struggle with palpitations related to mental health concerns may derive benefits from exercise, counseling or therapy, medications, or mindfulness apps, among other options. Importantly, if palpitations are related to mental health, they may never truly go away and discussions with your physician center more around living with the sensations than actually finding a way to get them to completely go away. However, once patients get reassurance from a thorough cardiac evaluation that their heart appears to be doing well, patients then often do better and have a better chance of success in attending to their mental health concerns. However, we lack data as to how paying too much attention to wearable technology may worsen pre-existing anxiety, so patients may benefit from discussing pre-existing anxiety and wearable technology with their physicians before purchasing expensive devices for the home.
Thyroid dysfunction, particularly hyperthyroidism, is seen in some individuals with troubling palpitations. There may be other endocrine-related issues to consider when evaluating for causes of palpitations. Consequently, your physician may want to order bloodwork as part of the evaluation for your palpitations.
What people drink has a significant influence on palpitations. Caffeine, other stimulants, some supplements, and alcohol can all potentially worsen palpitations. Caffeine consumption should generally be less than 200 mg/day and those struggling with palpitations often benefit from stopping ingesting any caffeine.
Wrapping it Up
As I mentioned earlier, it is best to start your evaluation of your palpitations with your physician to ensure you get evaluated for the rare, but potentially serious causes of palpitations. Many patients experience palpitations and are relieved to learn their heart is doing well. As with most other things, your body will respond well to adequate exercise, good quality sleep, less alcohol and caffeine, and a healthy diet, such as the Mediterranean Diet.
References:
Mannina et al. Int J Cardiol. 2021 Aug 15;337:64–70. doi:10.1016/j.ijcard.2021.05.006.
Torrado et al. J Cardiovasc Electrophysiol. 2025;36:54–61. doi:10.1111/jce.16478.
Williams et al. Heart. 2020;0:1–8. doi:10.1136/heartjnl-2020-316925.




Comments